2. THE FORMATIVE YEARS
2.4 The Tumkur district baseline studies
After having gained expertise in carrying out research field work at Kirangur and Bangalore, one of the most challenging assignments of the NTI was planning and execution of operational studies which had direct bearing on the proposed nationally applicable controlled programme. What preventive measures can be taken to break the chain of transmission? What were the likely steps involved? Which method is cost effective and efficient? Which agencies could be involved? Will this be simple and easy to understand by those who operate it and those who derive benefits? Can this be carried out without guidance from experts? Will it not demand a superstructure to maintain it? Will this be equally applicable anywhere in this vast country? Most important, will this be acceptable to the people, especially the rural uneducated poor? Will they be appreciative of the services rendered to improve their health? A core group of highly motivated scientists began working together. Even though national and international officers headed this programme, it did not recognise hierarchy. The questions that arose were not new. However, their concern to effectively solve them was new.
 Mr. S.S. Nair Sr. Statistical officer |
 Mr. G Ramanatha Rao Jr. Statistical officer |
The Bhore and the Mudaliar Committees13,37 had kept in view some of the queries related to free treatment, emphasis on preventive work, adequate health services to the vast population, etc. The Committees had suggested that the training of basic doctors should be designed to equip them for guiding the people to a healthier and happier life. Since Independence, the Indian government was run on democratic principles and community development was given a high priority. People’s participation in various schemes were being encouraged. In the health sector, the Mass BCG Campaign, National Malaria Eradication Programme (NMEP), and National Health and Family Welfare Programme (NHFWP) had created a general awareness among people. The experience from these programmes were utilised by the NTI. These led to the decision to base the operations taking the entire district into consideration. This was because the district was an administrative unit in India with recognised boundaries, divided into taluks, sub-divisions and villages. All states in India have districts. Census, revenue and other data were readily available, all linking to the district principle. Various departments of the government including the health department used this fundamental unit. Hence, it could be used in TB work too and standardised scientifically to be applicable elsewhere.
In selecting a district for doing the field work, Tumkur was the obvious choice. Tumkur was a district adjacent to Bangalore, with the headquarter town, just 70 kms away, on the highway NH4. It had all the characteristics of an average Indian district and majority of the population (88%) lived in 2,400 villages.
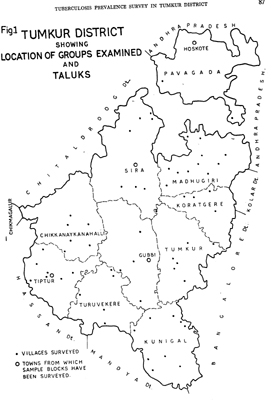 Tumkur District map with location of groups and taluks |
Among the first protocols written, was the one by EPS: RP/19 - A baseline TB prevalence survey in Tumkur district (Annexure II). This was a vital study providing accurate estimates of infection and disease prevalence. The information on prevalence of infection was not available from NSS as in that survey the population was not subjected for tuberculin testing. It should be noted that this was the first survey in India wherein, adopting the district as a unit, epidemiology work was done in a randomly selected population. It was to the credit of the teams that field work was completed in record time. The main findings are given in table on page no. 51.
| Male | Female | Total | |
| 1. De facto population | 16,283 | 15,684 | 31,967 |
| 2. Infection rate (%) [14 mm] |
33.5 | 28.5 | 30.9 |
| 3. Radiological prevalence rate (%) [based on two readers] | 2.5 | 1.2 | 1.9 |
| 4. Bacillary prevalence rate % (among X-rayed) | 0.56 | 0.25 | 0.41 |
Meanwhile, the Control Section (COS) developed several protocols (RP/22, 23, 24) had several sub-protocols, (Annexure II) covering case finding and treatment activities and for assessing the immediate results of the programme. The major protocol RP/21: Investigations of nationally applicable TB control programme, is of great historic importance.
To implement the tasks elaborated in the protocols, most of the resources of the NTI were mobilised and transferred to the camp office at the Tumkur District TB Clinic. It is to the credit of the GOM that a large portion of the District TB clinic premises was loaned to house the camp/field offices, free of cost. Field work began in April 1960. The studies continued till 1963. The problem-solving sessions were continually being attended by senior officers and field staff. Sometimes these sessions were held in the village where actual work was going on. Drs Piot and Baily were present, almost daily, to oversee different activities. Besides the regular NTI staff, services of the three BCG teams were utilised to optimise output of different types of activities. The enthusiasm was such that in the first three months, about 1,12,000 population was covered. By October, the following major operations research got under way:
a) A pilot phase was conducted in Beladhara Circle, Tumkur taluk. Here, case finding by mass campaign X-ray (MCX) was undertaken and cases identified were treated. This helped to gain experience in field problems for drawing up of the protocols of the operations research phases;
b) The first phase of operations research envisaged the mass campaign and community development approaches with X-ray [MCX and case detection X-ray (CDX)] and sputum [mass campaign sputum (MCS) and case detection sputum (CDS)] case finding. In the mass campaign approach (MCX and MCS) the BCG teams were utilised to refer tuberculin positive persons and all above the age of 40 for chest X-ray or for sputum examination offered in the villages. In the community development approaches (CDX and CDS), the community development personnel sent the symptomatic persons for X-ray or sputum examination.
The treatment of cases diagnosed by these four different approaches had been undertaken by four channels, viz., (i) the village panchayat chairman; (ii) gram sevak; (iii) primary health unit (PHU) and (iv) the NTI channel (HV from NTI). The first phase ran according to schedule from April 1961 to the middle of August 1961. The treatment of cases continued for a full year when their post-treatment assessment was made.
c) The second phase of the operations research programme started in September 1961. This phase was based on some of the experience gained in the first phase and keeping in view the feasibility of a control programme. The phase was planned with the four different approaches as envisaged in Phase I. As it was thought that the first phase was conducted in the low prevalence area, Phase II was implemented in the northern half of the Tumkur district which presumably had a higher prevalence. The essential differences in the case finding and treatment approaches in Phase I and Phase II consisted of:
i) In mass campaign approaches, symptoms were used as an additional screening test for case finding in Phase II as against only tuberculin reaction in Phase I. Tuberculin tests were given only in the age group 0-20 in Phase II as against all persons in Phase I, limiting the BCG vaccination also to 0-20 in Phase II. BCG vaccination was limited to tuberculin negatives in 0-40 in Phase I.
ii) In community development approaches, X-ray and sputum examination services were offered at a central point in Phase II as against in the villages in Phase I. The criteria for selection remained the same in Phase I and Phase II.
iii) The treatment in Phase I had been organised through the four channels enumerated above independently. In Phase II, all treatment had been offered through the PHU situated in the area of operation with different channels such as village panchayats, gram sevaks acting as subsidiaries to the PHUs. The community development programmes in Phase II had been planned so as to study long-term impact of a regular case finding facility offered within short distance in rural areas.
In the second phase, double drug (PAS+INH) therapy was
given to all sputum positive cases diagnosed either in the sputum or X-ray
case finding programmes and INH alone to others. In the first phase, INH
alone was available to all cases. The initial motivation in all the channels
was done by the NTI HVs (RP/24 Annexure II)
The analysis of the case finding results have revealed the following points
of operational relevance. The advantage of a tuberculin reaction in selecting
groups for further examination was outweighed by operational implications
of coverage and absenteeism at various stages. Awareness of symptoms among
positive cases could form the basis of a very efficient, integrated case
finding programme. The older age groups, where prevalence of radiological
cases was higher, neither responded favourably to direct motivation nor
attended X-ray centres (XCs) which were within walking distance.
To handle the enormous output from different areas of work efficiently, STAT established a field statistical unit at Tumkur comprising a Statistical Assistant (SA) and a statistical clerk to assist the field teams. This unit dispensed the precoded cards and forms on a daily basis and after completion of work, received them, checked these and the next day, arranged for their despatch to the NTI by the communication vehicle. In addition, the unit transferred the MMR X-ray results, direct smear results and maintained the treatment division where treatment was offered to persons diagnosed as a case in the survey. It also maintained the Daily log book for calculation of cost and assessment of transport efficiency.
Many types of operational research activities were initiated. For e.g. the new X-ray machines were field tested. MMR chest X-ray readings were underscored with an epidemiological bias and became more objective. Different readers were subjected to assessment under joint parallel reading and umpire reading. Every X-ray reader was evaluated and information recorded was standardised. Methodologies of collecting ‘spot’ (evening hours when field work was being done) and ‘overnight’ (whole night sample collected from the patient early next morning) sputum samples, their storage in the field, transportation to the laboratory at NTI, were worked out.
The Sociology Section (SOCS) had a highly motivated team of workers. Through operations research studies, they began to evaluate the level of awareness and action taken by patients, i.e. persons with chest X-ray shadows suggesting TB by two readers and persons whose sputum is positive by smear. These two are different concepts. Even in the west, clear indicators were not available because sociological concepts were not given serious weightage till then. Further, the concepts of the west, even if available, may not be applicable in India.
Research studies RP/29, 30, 32 and 34 (Annexure II) formed the basis of sociological considerations viz., community awareness, felt need and action taking of TB and qualitative assessment of operational investigations. The findings of these pathbreaking studies were fully incorporated in the Programme.
Words fail to describe the exemplary work carried out by field workers. Excerpts from the WHO quarterly reports36: With such a large part of the senior staff not in position, so much more responsibility is left on the shoulders of those who are present. It is wonderful to see how some of our staff, particularly the technicians, are taking on these increased responsibilities with a tremendous sense of duty. We have, for example, now four case finding programmes operating in Tumkur district with only one MO in charge. One senior health inspector heads each of these programmes. He carries out the planning and organisation of the work with all the assurance of a seasoned public health officer. If any one of our colleagues is feeling frustrated in New Delhi or Geneva, he should spend a couple of nights - as did our GOI Adviser in TB recently to see how the staff work. Come and see the community development approach where a Senior Health Inspector gets 200 villagers, who have converged from three or four villages with slips issued by their Panchayat Chairman, into an orderly queue under the big tree. The XT in a matter of 20 minutes gets tent, ropes, lighting, screens and X-ray unit in order to put the chairman as the first man on the patient list.
In the field programmes and at the NTI itself we have groups of excellent technicians doing work which is more often than not slightly more than what they are really expected to do. The staff are just that little better than they need be which makes all the difference. The WHO statistician says that our sorter-operator is the smartest man he has come across at a statistical machine . These people are the hard core of NTI and thanks to them NTI seems to grow into something that the government, the WHO and UNICEF can become proud of.
From the epidemiological, sociological and operations research studies, invaluable information was gathered. As Dr Baily summarises: (1) About half the patients suffering from TB did take action and go to the nearest health centre for relief. (2) Most of the self-reporting patients were not diagnosed as cases of TB , nor was further appropriate action taken. (3) Mass case finding in any other form bypassing this action taking pattern would yield very few cases. (4) The cost of diagnosis would be enormous and out of proportion to the probable cost of treating them by domiciliary chemotherapy38.
Based on the findings, a draft recommendation for the DTP was prepared in 1961, keeping in mind an average Indian district, its population and health facilities available39. Extreme care was taken to limit interference with the existing system, to augment shortfalls, if any, so that the TB control programme would be naturally absorbed within the system. For the first time, the application of operations research methodology was used in the field of general health. It is to NTI’s credit that this methodology which was hitherto used extensively in the field of industry or war was effectively used to reduce the suffering from a disease.
Detailed work manuals for the (i) District TB Officer (DTO); (ii) Treatment Organiser (TO); (iii) LT; (iv) SA; (v) XT; and (vi) Peripheral Health Institutions (PHIs) were prepared along with an introduction to the proposed DTP. A seminar held at NTI in 1962 was attended by senior TB officers from the GOI and from 12 different states40. (Annexure III, sl no.3). After obtaining approval of the concerned authorities, the first edition of the manuals were issued in 1962.
The national programme policy as enunciated in the introduction
manual of DTP (Annexure III, sl no.3) comprised:
• Domiciliary treatment
• Use of standard drug regimen
• Duration of treatment, 12-18 months
• Treatment free of cost
• Priority to newly diagnosed smear positive treated patients
• Treatment organisation fully decentralised
• Efficient defaulter system/mostly self-administered regimen
• Timely follow up
• Chemoprophylaxis not recommended as it is impractical
Perhaps nowhere else the problem of tackling TB was treated as a multi-dimensional problem. The problem and its determinants had been identified. Methods of intervention were scientifically worked out. For the first time, social sciences were consciously included as hard evidence and peoples’ voices were placed on par with science, technology and administration. The National Programme was fully integrated with the GHS of the country, thus extending the scope of TB work to be available through its vast reaches.